 Nightmares: We’re Not at Their Mercy
Nightmares: We’re Not at Their Mercy
By Antonio Zadra, PhD
 Because of their intense emotions and vivid, troubling imagery, nightmares have always been a source of fascination. Nightmares were observed by Hippocrates (the “father” of medicine) and are discussed in the Babylonian epic poem of Gilgamesh (2000–3000 BCE), the oldest great work of literature, about the most famous of all Assyro-Babylonian heroes.
Because of their intense emotions and vivid, troubling imagery, nightmares have always been a source of fascination. Nightmares were observed by Hippocrates (the “father” of medicine) and are discussed in the Babylonian epic poem of Gilgamesh (2000–3000 BCE), the oldest great work of literature, about the most famous of all Assyro-Babylonian heroes.
Nightmares are extremely dysphoric dreams involving threats to an individual’s emotional or physical sense of safety or threats to or loss of loved ones. They are common in children, adolescents, and adults. Approximately 5% to 8% of the general adult population reports having nightmares once per week or more often, and lifetime prevalence for nightmares is practically 100%. To be considered a “disorder,” nightmares need to cause significant daytime suffering and distress, while the term “chronic nightmares” is typically used when nightmares persist for at least six months with a frequency of one or more nightmares per week.
For the longest time, people believed that nightmares were due to strange or largely untreatable sources, such as the presence of demonic spirits, oxygen shortage (a pillow blocking the airway), or gastric disturbances during sleep (the pepperoni pizza hypothesis). In the beginning of the 20th century, nightmares were often viewed as a secondary symptom related to core, underlying psychological issues. For these reasons, nightmares were seen either as a problem which people were largely helpless to cope with successfully, or as a disturbance that would disappear only once the psychological issues at the root of the nightmare were uncovered and dealt with.
In the past few decades, a new view has emerged in dream science. A wealth of clinical studies have shown that simple and highly effective treatments for nightmares exist. Unfortunately, though, the idea that there is nothing much one can do about nightmares remains widespread in the general population. Moreover, only a minority of people with frequent nightmares ever seek help from a healthcare professional for their condition, and fewer than one-third of people who have frequent nightmares believe that nightmares are treatable.
Current best practice guides for the treatment of nightmares consistently recommend imagery rehearsal therapy (IRT) as the treatment of choice. IRT is a cognitive imagery intervention that teaches patients to change their remembered nightmares and to rehearse new scenarios. This approach has been successfully used in both children and adults, and in veterans, trauma victims, people living through major stressors or life crises, and patients suffering from serious mental illness, such as depression.
The main idea behind IRT is to have people “rescript” their nightmares in whatever way feels right to them, and then rehearse the new dream using visual imagery. Thus, whereas most people try to forget a nightmare as quickly as possible, now they are instructed to deal with the nightmare in a constructive and active way. Because clients are told to “change the dream any way you wish,” the focus of their change can range from the very beginning of the nightmare to its general theme to a detail like the setting or the color of a wall. Thus IRT does not incite people to necessarily focus on the nightmare’s ending or to transform the dream into something triumphant.
The key instructions for IRT typically include the following steps: (1) select a disturbing dream, preferably one of lesser intensity (with a less threatening nightmare, people usually find it easier to imagine and rehearse a changed version); (2) change this nightmare any way you wish; (3) rehearse this new dream a few minutes each day (twice can suffice) at a time of your choosing; and (4) continue these instructions every day, and consider working with a different nightmare every 3 to 7 days as needed. It is also vital to remind clients that they are to rehearse the new dream only, and not the nightmare. The treatment is relatively straightforward and highly effective, and adverse effects are rarely encountered.
Addressing nightmares can be all the more important because their negative aspects can go well beyond the distressing experiences they present in and of themselves. Increased frequency of nightmares is correlated with severe sleep disturbances, including higher rates of insomnia; increased severity of psychological and psychiatric distress; suicidal ideation; and poor physical health. By directly targeting nightmares, people can experience significant improvements not only in nightmare frequency, but also in these other spheres.
 So what causes nightmares? Many factors can be involved. Early traumatic experiences (abuse or psychological neglect, for example), life stressors (such as moving to a new city, divorce, financial worries, starting a new job), and genetics can all play a role. In some people, nightmares can be related to their personalities (people who are particularly sensitive or highly creative or artistic are among those who may be more prone to nightmares). Or nightmares can be triggered by medications (including some antidepressants, barbiturates, and beta blockers).
So what causes nightmares? Many factors can be involved. Early traumatic experiences (abuse or psychological neglect, for example), life stressors (such as moving to a new city, divorce, financial worries, starting a new job), and genetics can all play a role. In some people, nightmares can be related to their personalities (people who are particularly sensitive or highly creative or artistic are among those who may be more prone to nightmares). Or nightmares can be triggered by medications (including some antidepressants, barbiturates, and beta blockers).
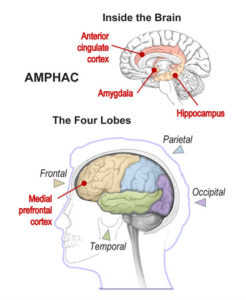
One recent neurocognitive model of nightmare production, known as AMPHAC (short for amygdala, medial prefrontal cortex, hippocampus, and anterior cingulate cortex – brain regions believed to be responsible for generating nightmares), suggests that variations in nightmare frequency and severity reflect the influence of two underlying factors: affect load, or day-to-day variations in emotional stress, and affect distress – a disposition to experience heightened distress and negative affect and to react with strong behavioral expressions. In AMPHAC and other models like it, nightmares are seen as resulting from a dysfunction in a brain-based network that, during normal sleep and dreaming, helps regulate emotions.
Finally, it is important to note that the occasional experience of nightmares is a normal and virtually universal human experience. Moreover, some people with nightmares have no interest in treatments, because they feel that nightmares form part of who they are or that they contribute something valuable to their general well-being. For those who are troubled by chronic or trauma-related nightmares, however, it is vital to know that there exist highly effective, non-pharmacological treatment options. In other words, nightmares may be a common experience, but they are not something we are helpless to act upon.
………………………………………………………………………………………………………………………….
© 2018 Antonio Zadra. Antonio Zadra, PhD, is a professor of psychology at the Université de Montréal (Canada) and director of the university’s Dream Laboratory. He leads a research group investigating non-REM sleep parasomnias at the Center for Advanced Research in Sleep Medicine. His research focuses on the relation between dream content and waking experiences, the correlates and treatment of dream-related disorders, and the pathophysiology of sleepwalking.
Banner images: (Center) Pixabay/EriktheGreat, CC0. (Left) Plate 1. Sir Charles Bell, The anatomy of the brain, 1802. Wellcome Collection, CC BY.
The International Association for the Study of Dreams is a nonprofit, international, multidisciplinary organization dedicated to the pure and applied investigation of dreams and dreaming. Our members variously explore dreams through the sciences, the humanities, the arts, clinical applications, and their own experiences. See our website (ASDreams.org) for information on dream research, research grants, membership, and conferences. IASD is a partner in the global Brain Awareness Week campaign of the Dana Alliance, which offers a large selection of brain education materials on its website (dana.org/baw).
